Accidentally injecting air into a muscle can lead to an “air embolism,” which can be serious. The consequences depend on factors like the amount of air and the blood vessels involved:
- Minor cases may cause localized discomfort and swelling.
- Larger amounts of air can lead to an air embolism, potentially causing symptoms like dizziness, chest pain, and even loss of consciousness.
- However, if air reaches the lungs, it can cause a pulmonary embolism, a medical emergency with symptoms like shortness of breath and chest pain.
- Air emboli in the brain or coronary arteries can result in strokes or heart attacks, which can be life-threatening.
How does the body handle small air in muscles?

It’s important to note that minor symptoms resulting from small air injections are typically not a cause for concern. However, healthcare professionals take precautions to minimize the risk of air entering the bloodstream during injections.
Description of minor symptoms for small air injections
When a small amount of air is injected into a muscle, it may result in localized discomfort or pain at the injection site. This pain is typically mild and may be described as a dull ache or a sensation of pressure.
Furthermore, some individuals may experience mild swelling at the injection site. This occurs due to the body’s natural response to the presence of foreign substances, including air, in the muscle tissue. The swelling is usually not severe and tends to resolve on its own over time.
In some cases, the injection site may become slightly red and warm to the touch. This is another common response to irritation caused by the presence of air, but it is generally not a cause for alarm.
How the body can handle small amounts of air
The human body is capable of absorbing small amounts of air without causing major harm. When a small air bubble is introduced into the muscle tissue, the surrounding blood vessels and tissues can gradually absorb and eliminate the trapped air.
In addition, the circulatory system plays a role in transporting the air to the lungs, where it can be expelled through exhalation.
In many cases, the minor symptoms resulting from a small air injection will self-resolve over time. The body’s natural healing processes work to minimize discomfort, swelling, and inflammation. Adequate hydration and gentle movement of the affected muscle can help facilitate this process.
Small amounts of air in the bloodstream are generally not clinically significant or dangerous. The human body has mechanisms in place to prevent air from causing serious harm when introduced in small quantities.
What are the symptoms of an air embolism?
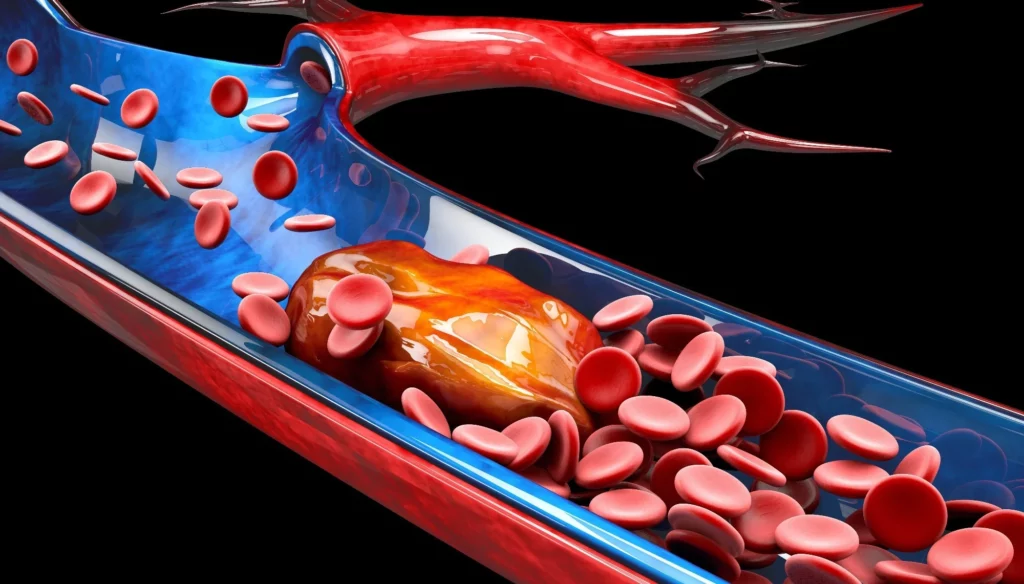
An air embolism is a medical condition that occurs when air or gas enters the bloodstream, forming an embolus (a blockage). This blockage can obstruct the flow of blood through blood vessels, leading to potentially serious consequences.
Air embolisms can occur when air enters veins or arteries, and they can travel to various parts of the body, including the brain, heart, lungs, or other vital organs.
Symptoms and severity of air embolisms
The symptoms and severity of an air embolism can vary depending on factors such as the amount of air introduced and where it lodges in the circulatory system.
Common symptoms of an air embolism may include:
- Dizziness and lightheadedness
- Rapid heart rate (tachycardia)
- Shortness of breath
- Chest pain or discomfort
- Cyanosis (bluish discoloration of the skin)
- Altered mental status, confusion, or loss of consciousness
- Weakness or paralysis, especially if the embolism reaches the brain
- The severity of an air embolism depends on factors like the size and location of the embolus. Small emboli may cause milder symptoms, while larger ones can lead to more serious complications.
Potential complications and risks
If the air embolism reaches the lungs, it can cause a pulmonary embolism, which is a blockage in the pulmonary arteries. This condition can result in severe chest pain, difficulty breathing, and even cardiac arrest.
When air emboli travel to the brain and block blood flow, they can cause a stroke. Stroke symptoms may include sudden weakness, numbness, difficulty speaking, and loss of coordination.
In some cases, air embolism can block coronary arteries, leading to a heart attack. Symptoms of a heart attack include chest pain, shortness of breath, and nausea.
Prolonged blockage of blood flow to organs can lead to tissue damage and organ dysfunction. The severity of organ damage depends on how quickly the embolism is identified and treated.
In severe cases, untreated air embolisms can be fatal, particularly if they block critical blood vessels supplying vital organs.
How does air cause a pulmonary embolism?
A pulmonary embolism (PE) occurs when an embolus, typically a blood clot, but in this context, potentially air or gas, travels through the bloodstream and becomes lodged in the pulmonary arteries, which supply blood to the lungs.
In the case of air embolism, it means that air has entered the bloodstream and traveled to the pulmonary arteries. This can happen when air is accidentally introduced into a vein, and it is carried through the circulation to the lungs.
Symptoms of pulmonary embolism:
The symptoms of a pulmonary embolism can vary in severity, and they often develop suddenly. Common symptoms include:
Sudden Shortness of Breath: This is typically the most prominent and alarming symptom. Patients often experience rapid and labored breathing.
Chest Pain: Chest pain, which can range from sharp to a dull ache, is another common symptom. It may worsen with deep breaths or coughing.
Coughing: Some people with PE may cough up blood or bloody sputum.
Rapid Heart Rate (Tachycardia): The heart rate increases as the body tries to compensate for decreased oxygen levels in the blood.
Leg Swelling and Pain: In some cases, PE can be associated with deep vein thrombosis (DVT), where blood clots form in the legs. This can cause leg swelling and pain.
Feeling Lightheaded or Fainting: Reduced blood flow to the heart can lead to dizziness and even loss of consciousness.
It’s important to note that some individuals may not exhibit all of these symptoms, and the severity of symptoms can vary widely.
Urgency and life-threatening nature of a pulmonary embolism
A pulmonary embolism is a medical emergency and is considered life-threatening. The urgency stems from the fact that it can severely compromise the ability of the lungs to oxygenate the blood, leading to hypoxia (low oxygen levels) and potentially cardiac arrest.
If not promptly treated, a large or multiple emboli in the pulmonary arteries can be fatal. Even in cases where it doesn’t result in immediate death, a PE can cause long-term complications, including damage to the lung tissue and increased risk of recurrent embolisms.
Immediate medical attention is crucial when a pulmonary embolism is suspected. Treatment typically involves anticoagulant medications to prevent further clot formation and sometimes procedures like thrombolytic therapy or surgical removal of the embolus.
Early intervention can significantly improve the prognosis, but delays in diagnosis and treatment can be life-threatening. Therefore, recognizing the symptoms and seeking medical help quickly is of utmost importance.
Can air emboli cause strokes and heart attacks?
Air emboli can lead to strokes and heart attacks when they travel to and block the arteries supplying blood to the brain or heart, respectively.
In the case of a stroke, when an air embolism obstructs a cerebral artery, it reduces or completely cuts off blood flow to a portion of the brain. Without an adequate supply of oxygen and nutrients, brain cells begin to die, leading to neurological deficits or even death.
When an air embolism blocks a coronary artery supplying the heart muscle, it can result in a heart attack (myocardial infarction). The heart muscle becomes deprived of oxygen and begins to die, which can lead to various cardiac complications.
Symptoms of stroke and heart attack due to air embolism
The symptoms of a stroke or heart attack caused by an air embolism are similar to those of strokes or heart attacks resulting from other causes, but they can occur suddenly and without warning.
Symptoms of a stroke may include
- Sudden weakness or numbness, typically on one side of the body.
- Difficulty speaking or slurred speech.
- Sudden severe headache.
- Loss of coordination or balance.
- Visual disturbances, such as blurred vision or loss of vision in one eye.
Symptoms of a heart attack may include
- Severe chest pain or discomfort that may radiate to the arms, neck, jaw, or back.
- Shortness of breath.
- Nausea or vomiting.
- Cold sweats.
- Lightheadedness or fainting.
How do professionals prevent air embolisms in injections?
Healthcare professionals, including nurses and physicians, are trained to follow strict injection guidelines for several crucial reasons:
Patient Safety: The foremost concern is the safety and well-being of the patient. Following guidelines ensures that injections are administered in a way that minimizes risks, including the risk of air embolism.
Medical Efficacy: Proper injection techniques are essential for the effectiveness of medical treatments. Medications need to be delivered accurately to the intended target, whether it’s a muscle, vein, or other tissue.
Minimizing Complications: Adhering to guidelines helps prevent complications such as infections, tissue damage, or, as in the context of this discussion, air embolisms.
Professional Standards: Healthcare professionals are held to high standards of practice and ethics. Following established protocols and guidelines is not only a legal requirement but also an ethical obligation.
Steps to prevent air embolisms during injections
To prevent air embolisms during injections, healthcare professionals take specific precautions and follow established best practices:
Removing Air Bubbles: Before administering an injection, healthcare providers carefully remove any air bubbles from the syringe to ensure that only medication or fluid is injected.
Proper Needle Insertion: Healthcare professionals are trained to correctly insert the needle into the chosen tissue (e.g., muscle or vein) to minimize the risk of introducing air into the bloodstream.
Aspiration: In the case of intravenous (IV) injections, healthcare providers often aspirate (draw back on the syringe) to check for blood return before injecting medication. If air is accidentally aspirated, it is discarded, and the procedure is reattempted.
Secure Needle Attachment: Properly securing the needle to the syringe and ensuring there are no leaks or disconnections during the injection process is critical.
Monitoring: Healthcare providers closely monitor the patient during and after injections for any signs of complications, including immediate recognition of potential air embolisms.
The significance of seeking immediate medical attention if an air embolism is suspected
If a patient or healthcare provider suspects that an air embolism has occurred, seeking immediate medical attention is of paramount importance:
Early Intervention: Early intervention is crucial to prevent the embolism from causing further harm. Timely treatment can reduce the size and impact of the embolism.
Diagnostic Confirmation: Healthcare professionals can confirm the presence of an air embolism through diagnostic tests such as ultrasound, CT scans, or echocardiography.
Treatment Options: Medical treatments may be administered to address the embolism, such as positioning the patient to prevent the embolism from traveling further, providing oxygen, and sometimes using medications or procedures to remove the air from the bloodstream.
Preventing Complications: Early intervention can help prevent complications such as stroke, heart attack, or organ damage associated with air embolisms.
FAQ’s
What happens if you inject 1 ml of air?
Injecting a small amount of air (1 ml) into the muscle or under the skin is generally not harmful and is unlikely to cause any significant medical issues. However, it’s best to avoid injecting air whenever possible to minimize any potential risks.
Are air bubbles in intramuscular injections lethal?
Small air bubbles in intramuscular injections are generally not lethal. They may cause discomfort or minor issues, but severe complications from small air bubbles are rare.
How much air is too much to inject?
The amount of air that is considered “too much” to inject varies depending on the specific situation and patient. In general, healthcare professionals take precautions to avoid injecting significant amounts of air into veins, as this can potentially lead to air embolism, which can be dangerous.
How much air is OK in a syringe?
It is generally considered safe to have small air bubbles in a syringe when administering injections, especially subcutaneous or intramuscular ones. However, healthcare providers often try to expel air bubbles to ensure accurate dosing.
What happens if a small air bubble is injected into veins?
Injecting a small air bubble into a vein is usually not harmful, as the body’s circulation can often dissipate small amounts of air without causing serious issues. However, larger volumes of air can potentially lead to an air embolism, which can be a medical emergency.
Does air embolism go away?
Small air embolisms may resolve on their own as the body absorbs the trapped air. However, large or serious air embolisms may require immediate medical intervention, such as aspiration of the air or other treatments to prevent complications.
Final Words
In conclusion, when it comes to accidental injections of air into the body, it’s essential to remember a few important things. Healthcare professionals follow strict guidelines to keep patients safe during injections. They take out air bubbles from the syringe, insert needles carefully, and monitor for any problems.
But if you ever suspect that an air embolism has happened, don’t wait. Seek help right away! Air embolisms can be very serious and even life-threatening. Getting prompt medical attention is the key to preventing complications. So, remember, safety first, and if in doubt, reach out for help.

